Table of Contents
Introduction - Peripheral Vascular Disease (PVD)
Have you ever been told that you have poor circulation? Your restricted blood flow could be the sign of a more severe medical condition called Peripheral Vascular Disease (PVD).
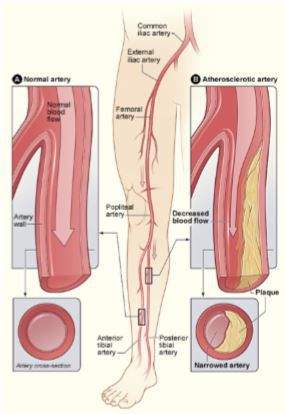
PVD is a broad term for any disease that impacts the blood vessels away from the heart. This can include arteries, veins, and in some cases, lymph vessels. The arteries and veins away the heart (periphery) are vulnerable to damage.
PVD is primarily split into two types: Peripheral Arterial Disease (PAD) and Chronic Venous Insufficiency (CVI). Both are serious and can make healing lower extremity wounds more difficult. When wounds have a hard time healing, you are at a bigger risk of infection, which in the worst-case scenario, could lead to amputation.
To reduce the risk of infection, diagnosing and treating your poor circulation is vital.
Diagnosing Peripheral Vascular Disease
A podiatrist is the right doctor to diagnose PVD because of how much it impacts your feet, ankles, and lower legs.
Your doctor will begin diagnosing PVD by doing a visual and hands-on exam of your lower extremities and reviewing your medical history. During the exam, your podiatrist will evaluate your pulse, skin condition, and look for any type of foot or lower limb deformities.
If the podiatrist believes that you might have PVD, you may be asked to go through a series of tests.
- Ankle-Brachial Index (ABI): a test that measures and compares your blood pressure in your arms and ankles. Measurement called “Waveforms” are also included.
- Doppler Ultrasound: a test used to assess blood flow, blockages such as clots or plaques, and to inspect the valves of larger veins.
- Angiography: is an X-ray or MRI imaging test used with a contrast dye to study your blood vessels in your legs, ankles, and feet.
The tests are done in an office or minor procedure room. If you are at risk of PVD, having these tests done is vital so you can move forward with treatment and minimize the impact PVD will have on your health.
Treatment for Peripheral Vascular Disease
Your podiatrist may recommend a specific treatment plan based on how severe your PVD is. In general, there are three main types of treatment for PVD available.
- Lifestyle changes. Simple: If you smoke, have a poor diet, or live a sedentary lifestyle, your podiatrist will recommend you change your living habits. This is recommended regardless of how advanced your PVD is.
- Medication. Your doctor might prescribe medication to improve your blood flow or control your blood pressure. Other medications that help lower cholesterol, control blood glucose levels, or prevent blood clots may also be prescribed. It’s important to have your primary physician, cardiologist, or vascular specialist involved with managing your prescription medications.
- Surgery. In some cases, a patient may need to referred to a specialist that performs vascular procedures of the lower extremities. With advancements in technology, this process has become significantly less invasive and much safer than ever.
If you believe you might have a type of PVD, it is critical that you seek help. Getting help and/or direction from a trained podiatrist may prevent more serious complications of PVD.
At Artisan Foot and Ankle Specialists, we diagnose PVD on a regular basis. We understand what to look for, and how to get you the treatment you need so that you can live a healthier and happier life. Call us today to schedule your consultation and find out if you may be at risk for PVD.