Table of Contents
Introduction
Ankle articular cartilage damaged through a single or multiple twisting injuries has limited ability for repair. This results in persistent joint-line pain, and persistent inflammation with weight-bearing activities. Loose fragments from the joint may float and produce occasional locking symptoms. Long standing severe damage to the articular cartilage can lead to debilitating osteoarthritis, which ultimately may require a joint replacement or fusion. For small lesions, current therapeutic options include monitoring, physical therapy, injections, and perhaps arthroscopic treatment. The arthroscopic treatment involves removing any loose fragment of bone and manually stimulating the injury area with micro-tools to promote active bleeding (called microfracture or abrasion arthroplasty). This will allow for the body to “patch” the area with a type of scar tissue called fibrocartilage.
For larger lesions an open procedure is necessary to resurface the damaged cartilage defect. This is necessary to slow the progression of arthritis that can spread over the rest of the joint surface. Resurfacing may involve cartilage grafting from a donor graft that is obtained from a certified bone graft, this often is from a refrigerated graft that keeps the cartilage cells alive while the bone is screened for disease. There are several techniques that are used to replace the cartilage. This can involve a block graft or a series cylindrical plugs called mosaicplasty or OATS procedure. The cylindrical plugs use an apple-corer like instrument to create a socket in the patient and another tool to harvest a precise cylinder to match the socket size from the donor bone. The goal is to produce a smooth gliding articular surface of hyaline or hyaline-like cartilage in weight-bearing surfaces of the ankle. By restoring the cartilage surface, weight-bearing function can also be restored and the progression of advanced arthritis to the remaining joint can be slowed.
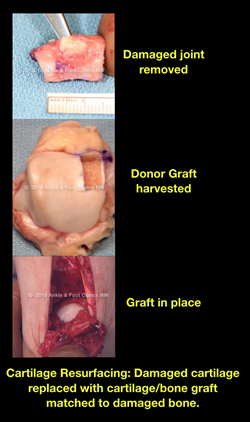
Warning - Graphic Image. Hover your mouse over image to see full-resolution version