Table of Contents
What Is PTTD?
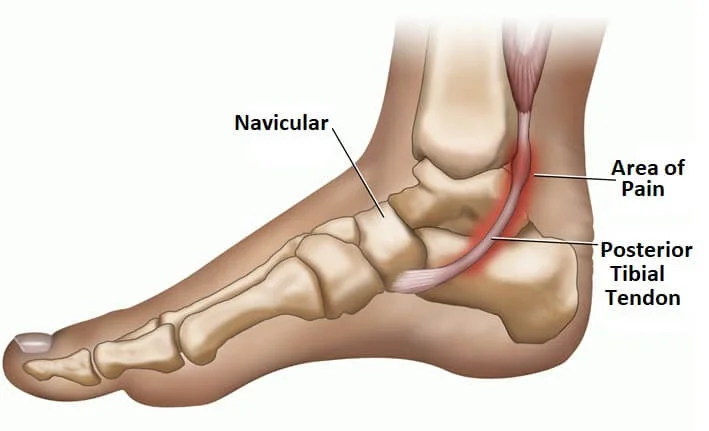
The posterior tibial tendon serves as one of the major supporting structures of the foot, helping it to function while walking. Posterior tibial tendon dysfunction (PTTD) is a condition caused by changes in the tendon, impairing its ability to support the arch. This results in flattening of the foot.
PTTD is often called adult acquired flatfoot because it is the most common type of flatfoot developed during adulthood. Although this condition typically occurs in only one foot, some people may develop it in both feet. PTTD is usually progressive, which means it will keep getting worse, especially if it is not treated early.
Causes
Symptoms
The symptoms of PTTD may include pain, swelling, a flattening of the arch and an inward rolling of the ankle. As the condition progresses, the symptoms will change.
For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm and swollen.
Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward.
As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably, and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
Nonsurgical Treatment
Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery, and progression of your condition can be arrested.
In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle and increasing limitations on walking, running or other activities.
In many cases of PTTD, treatment can begin with nonsurgical approaches that may include:
- Orthotic devices or bracing. To give your arch the support it needs, your doctor may provide you with an ankle brace or a custom orthotic device that fits into the shoe.
- Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weightbearing for a while.
- Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization.
- Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation.
- Shoe modifications. Your doctor may advise changes to your existing shoes, buy new shoes altogether, or prescribe special inserts designed to improve arch support.